Though it continues to pose a threat to the wellbeing of women and girls across the world, the fight against cervical cancer in Sierra Leone remains a challenge due to many factors including the lack of knowledge, late diagnoses and preventive mechanisms.

Cervical cancer according to the country’s health officials is the second most common cancer in women and girls between the ages of 15 – 45 in the West African country with an estimated population of eight million, with women accounting for fifty per cent of that population.
Speaking at a press conference last September, the Manager for the Expanded Programme on Immunization (EPI) Dr Desmond Maada Kangbai said three hundred and seventy- two (372) deaths were recorded of women suffering from cervical cancer in Freetown in 2020, and that Five hundred and fifteen (515) new cases are being detected annually.
“That tells us that the case fatality rate of cervical cancer in Sierra Leone is very high”, the doctor stated.
Global perspective
Cervical cancer is the fourth most common cancer globally, with about 600,000 annual cases. In Sub-Saharan Africa, which accounts for around 85% of the global disease burden, cervical cancer is the second most common cancer and the one responsible for the highest number of deaths, with 117,316 yearly cases.
The situation in Sierra Leone reflects this sub-regional reality. A national Cancer Registry was launched in 2012 but is now dysfunctional. Data collected from other sources indicate that even though cervical cancer is the second most prevalent cancer (after breast cancer), it’s the biggest killer of all cancers among women between 15-40 years. It also shows that approximately 500 cases are recorded annually, with an estimated 400 deaths every year.
In a study published in September 2022, “Case study of cervical cancer prevention in two sub-Saharan African countries: Rwanda and Sierra Leone,” written by Mohamed S. Bangura, et al, in Frontiers in Medicine, “Sierra Leone lags behind in terms of almost all cervical cancer prevention programmes.
Therefore, Sierra Leone needs more efforts to implement cervical cancer intervention programmes at the national level, including HPV vaccination.” Rwanda and Sierra Leone represented the best and worst cervical cancer prevention programme implementation in sub-Saharan Africa, respectively. Other sub-Saharan African countries mostly fall between these two countries.
Interestingly, in Rwanda, there was an impressive decrease in cervical cancer incidence in recent years. Rwanda achieved 93.3% human papillomavirus (HPV) vaccination of the three doses used in vaccinating girls in class 6 of primary school.
The solution
In an effort to eliminate this threat against women and girls in the country, the government through the Ministry of Health and Sanitation (MoHS) rolled out a vaccination exercise which lasted from the 3rd to 9th of October 2022 for 10-year-old girls who are mostly not sexually active.
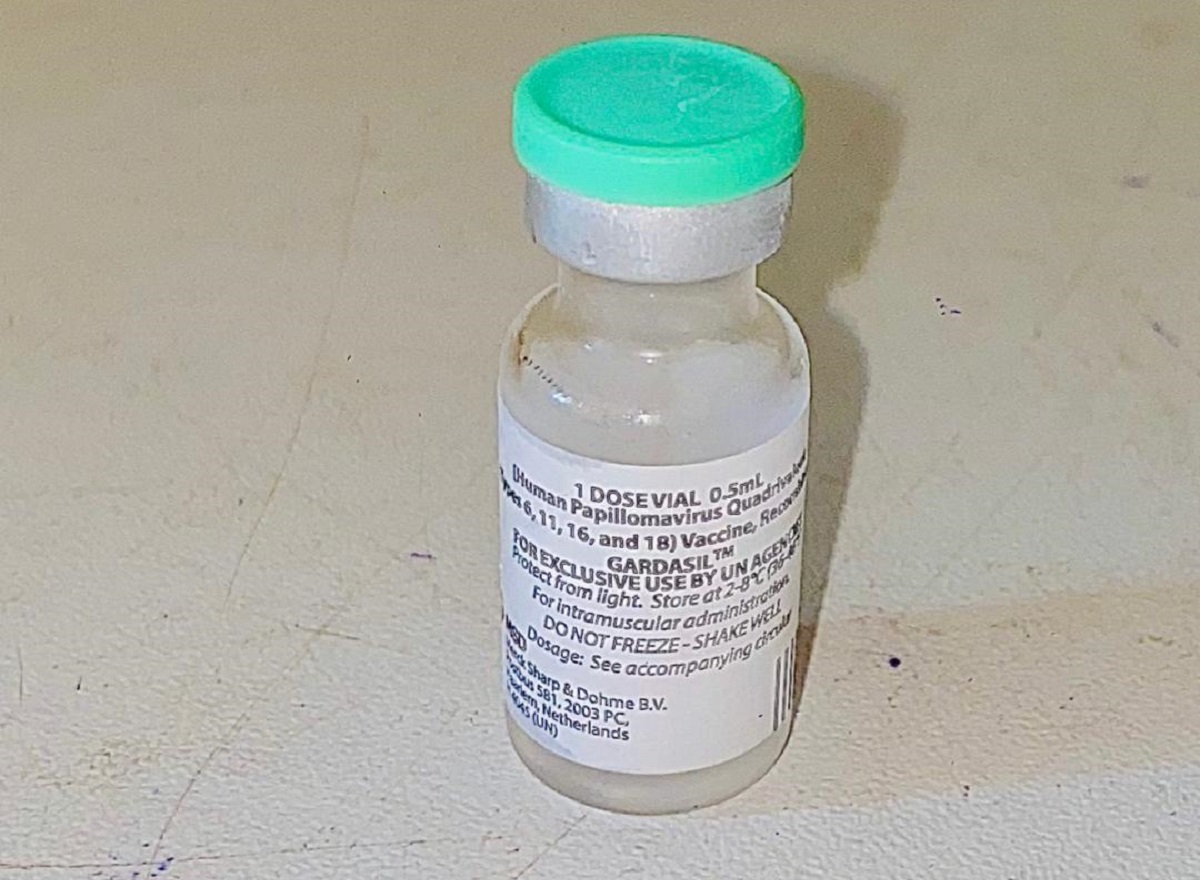
Medically known as the Human Papilloma Virus (HPV), its vaccine application was supported by the Vaccine Alliance of Gavi, the United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO).
A total of 153,991(one hundred and fifty-three thousand, nine hundred and ninety-one), girls, were given the vaccine, according to MoHS.
Alongside the Ministry of Basic and Secondary School Education (MBSSE), the campaign targeted 10 to 12-year-old girls in their last three years of primary school- classes 4-6.
According to the 2021 Annual School Census Final Report, released in June 2022, there were 383,405 girls in classes 4-6, in Sierra Leone. The HPV vaccine reached approximately 40 percent of eligible girls but there was no attempt to reach out-of-school girls, estimated at around 3,000.
Dr Mustapha Kabba, Sierra Leone’s Deputy Chief Medical Officer Bombali District, said they target young girls because they are most likely not to have started sexual intercourse that could have exposed them to the virus that causes cervical cancer.
Both COVID and the HPV vaccines would be given to girls, boys and women as a multiple immunization. “We want to ensure by the time the girls are fifteen years, 90% of them would have received the HPV vaccine,” he said.
The HPV vaccinations were initially meant to be given in two doses, but the second dose was dropped in April 2023. “After consultations with partners, including WHO, in fact, one dose can provide life-long immunity… long life protection. So, there is no need to give a second dose. This is new information,” said Umu Hawa Barrie Jalloh, a social mobilization officer with the Child Health, Extended Programme for Immunization (EPI) at the MoHS.
At the government-assisted St Joseph’s Primary School for girls in Makeni, Nesmanatu Koroma, a class six pupil, said the nurse asked her age and said she should contact her mother.
“I asked my mother and my mother said ‘yes’. Then, they injected me in the hand.” Following the injection, little Nesmanatu was given a pink card to show her mother.
Whilst the head teacher at a private school, Dwight International school in Makeni, Mohamed D. Jalloh refused to accept the vaccination process in his school stating that it was not of their knowledge as an administration, meanwhile he pleaded with them to check back later while he inform the parents though the feedback from parent after communication denied and frankly waned the principal not to allow their children to take the vaccine because they were not notified. He added.
“In Sierra Leone, we piloted the vaccine some years back but since then we have been unable to fully roll out the vaccine,” said Desmond Maada Kangbaui, Child Health and Expanded Programme for Immunization Manager.
Kangbaui said cervical cancer is the most frequent cancer among women in Sierra Leone and the second most frequent cancer among women around 45 years old. He said based on the data on cervical cancer, 515 new cases were detected in 2020, and 372 deaths reported. “This tells us that the case of the death rate in Sierra Leone is very high,” he affirmed.
According to the WHO, “Vaccination of adolescent girls is the most effective long-term intervention for reducing the risk of developing cervical cancer.”
HPV vaccines
The first HPV vaccine approved by the US Food and Drug Administration (FDA) in 2006, was manufactured by pharmaceutical giants GlaxoSmithKline and Merck & Co. It is worth mentioning that the Nobel Prize for Medicine in 2008 went to the German doctor Harald zur Hausen of the University of Düsseldorf for discovering the human papilloma virus that causes cervical cancer.
During the 1970s, Hausen found specific HPV-DNA in cervix cancer biopsies and thus discovered the new, tumourigenic HPV16 type in 1983. And in 1984, he cloned HPV16 from 18 (eighteen) patients with cervical cancer. HPV types 16 and 18 were consistently found in about 70% of cervical cancer biopsies throughout the world.
The global public health burden attributable to human papilloma viruses is considerable. More than 5% of all cancers worldwide are caused by persistent infection with this virus. Of the more than 100 HPV types known, about 40 infect the genital tract and 15 of these put women at high risk for cervical cancer. In addition, HPV is found in some vulval, penile, oral and other cancers. Human papillomavirus can be detected in 99.7% of women with confirmed cervical cancer, affecting some 500,000 women per year.
The role of HPV vaccination as a primary cervical cancer prevention method has been illustrated in numerous medical studies, including an observational study-“The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence,” written by Milena Falcaro, PhD, Alejandra Castañon, PhD, Busani Ndlela, PhD, et al. published in the Lancet Medical Journal on November 03, 2021.
This study showed 87% reduction in cervical cancer incidence and a 97% reduction in grade 3 cervical intraepithelial neoplasia incidences in women aged 20–29 years who were offered the vaccine at age 12–13 years as part of the national HPV vaccination programme in England. Because HPV is such a prevalent sexually transmitted virus, researchers and healthcare professionals specifically target girls and boys before they experience their first sexual contact.
Infection by the human papillomavirus is the most common sexually- transmitted disease, afflicting 50-80% of the population, according to the WHO.
Cervical cancer originates in a woman’s cervix, which connects the uterus to the vagina. According to the World Cancer Report released in April 2023, cervical cancer is the second largest cancer threat to women after breast cancer. The primary cause of precancerous and cancerous cervical lesions is infection with a high-risk or cancer-causing Human Papilloma Virus (HPV).
In a 2018 speech WHO Director Dr Tedros Adhanom Ghebreyesus, said “HPV vaccines are truly wonderful inventions.” The WHO Director-General, quoted a WHO report, Global Strategy to accelerate the Elimination of cervical cancer as a public health problem, that says: “Through cost-effective, evidence-based interventions, including human papillomavirus vaccination of girls, screening and treatment of precancerous lesions, and improving access to diagnosis and treatment of invasive cancers, we can eliminate cervical cancer as a public health problem and make it a disease of the past.”

This report was supported by the International Women’s Media Foundation (iwmf.org), Global Health Reporting Initiative: Vaccines and immunization in Africa.
ABOUT THE AUTHOR
Edna Ngegba is a dedicated and award-winning female Journalist in Sierra Leone who has made her mark in reporting on human rights and gender issues.
She is currently the Northern regional chairperson of Women in the Media Sierra Leone. She is currently the Nothern regional chairperson of Women in the Media Sierra Leone [WIMSAL]












Wow.! Impressive work done Edna